-
Breathe Clean: Better Informed is Better Protected



Breathe Clean: Better Informed is Better Protected
The 3M™ Molecular Detection System uses Isothermal DNA Amplification and Bioluminescence Detection to provide a simple means of detecting pathogens in food and environmental samples.
Breathe Clean: Better Informed is Better Protected
The 3M™ Molecular Detection System uses Isothermal DNA Amplification and Bioluminescence Detection to provide a simple means of detecting pathogens in food and environmental samples.
Breathe Clean: Better Informed is Better Protected
-
Airborne particles, mists thick with pollutants (PM 2.5/PM10), noxious gases - the air we breathe is becoming a bigger hazard to our health. Making an informed choice while choosing a respirator is critical, so that you are better protected in these adverse current conditions. 3M applies science to provide respiratory protection to help you breathe clean and filtered air, while keeping the pollutants at bay.
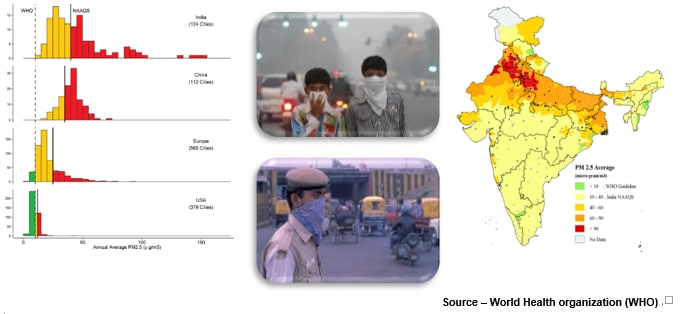
In the cities of developing nations, outdoor air pollution does not meet the World Health Organization (WHO) standards for acceptable pollutant levels. Risks of stroke, heart disease, lung cancer, chronic and acute respiratory diseases (including asthma) have increased, with nearly 3.5 million people dying due to these diseases every year. Moreover, 13 of the top 20 most polluted cities in the world are in India.
Particulate Matter (PM2.5), refers to particles in the air that cause pollution. These particles are released from a variety of sources, both indoors and outdoors. Although the atmosphere will always have PM2.5, certain levels are considered dangerously high. On an average PM2.5 reduces the life expectancy of humans by almost 3.5 years. The deaths in India over the last 5 years due to air pollution have increased by 15%.
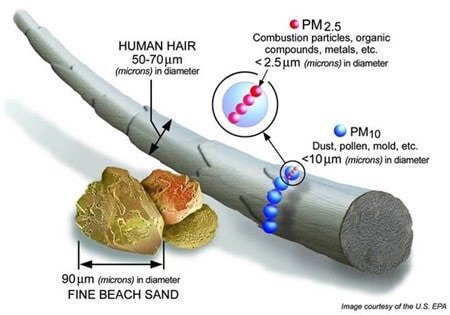
Why is it called PM2.5?
The ‘2.5’ in PM 2.5 refers to the size of the pollutant in micrometres. Particulate pollutants vary in size and the smaller they are, the more damage they cause to your health. Particulates that have a diameter of 10 micrometres or less are called PM10. Dust particles are the main source of PM10. Particulates that have a diameter of 2.5 micrometres or less are called PM2.5. These particles are so small that they can only be viewed under a microscope. Their small size makes them deadlier than PM10.
Where does PM2.5 come from?
• Combustion in vehicles and machinery
• Industrial processes, particularly those involving coal
• Emissions from power plants
• Chemical processes in the atmosphere which happen when gases and other pollutants from power plants react
• Sources inside the home, such as candles, lamps and fireplaces
• Vehicle emissions
• Bursting of firecrackers during festivals
• Forest fires and coal burning
What are the negative effects of exposure to PM 2.5?
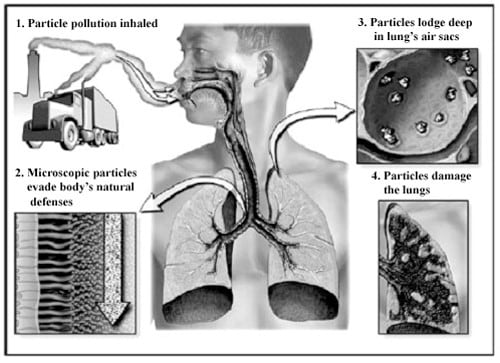
PM2.5 (with a size one-hundredth the thickness of a human hair) is produced by the incomplete combustion of fossil fuels and biomass. It can penetrate deep into the lungs and blood stream, and is dangerous at any concentration.
n 2013, IARC (International Agency for Research on Cancer) concluded that air-pollution is carcinogenic to humans. Another critical air-pollutants is ground-level ozone (O3) which not only damages human health but also crops. The exact sources of emissions must be assessed, which has currently only been done in a handful of cities, and a market-oriented approach must be implemented. A prerequisite to combating PM2.5 air pollution is a precise and comprehensive analysis of the emissions sources. India has a pollution level standard in place but a stronger enforcement of this law is the need of the hour.
Mounting evidence suggests that air pollution contributes to the large global burden of respiratory and allergic diseases including asthma, chronic obstructive pulmonary disease, pneumonia and possibly tuberculosis. Although associations between air pollution and respiratory disease are complex, recent epidemiologic studies have led to an increased recognition of the emerging importance of traffic-related air pollution in both developed and less-developed countries, as well as the continued importance of emissions from domestic fires burning biomass fuels primarily in the less-developed world. Emissions from these sources lead to personal exposures to complex mixtures of air pollutants that change rapidly in space and time due to varying emission rates, distances from source, ventilation rates and other factors. Although the high degree of variability in personal exposure to pollutants from these sources remains a challenge, newer methods for measuring and modelling these exposures are beginning to unravel complex associations with asthma and other respiratory disease. These studies indicate that air pollution from these sources is a major preventable cause of increased incidence and exacerbation of respiratory disease.
How can I protect myself against PM2.5?
n many areas of the world, concentrations of ambient air pollutants exceed levels associated with increased risk of acute and chronic health problems. While effective policies to reduce emissions at their sources are clearly preferable, some evidence supports the effectiveness of individual actions to reduce exposure and health risks. Personal exposure to ambient air pollution can be reduced on high air pollution days by staying indoors, reducing air infiltration to indoors, using air filters and limiting physical exertion, especially outdoors and near air pollution sources. Evidences have also suggested that the use of respirators (as opposed to masks) will be effective in such circumstances. However it is essential to have an awareness of the difference between Masks and Respirators.
Masks are more like a sieve-like structure which would prevent bigger particles to be stopped while smaller particles (anything less than PM10) would still pass through. The word surgical mask or mask (which normally people use in a PM 2.5 situation) would not serve any purpose. Only respirators should be used to prevent the effects from inhaling PM2.5.
Note that loose-fitting masks (e.g. gauze or surgical masks) are not considered respirators and do not provide much benefit in reducing exposure to airborne particles, because they typically have gaps between the face and the edge of the mask that allow leakage of air and particles into the mask (and thus the user’s respiratory system). Surgical masks were designed to protect the surrounding environment from the user’s own spit or mucous. Healthcare professionals use them (e.g. in an operating theatre) to prevent their own germs from infecting the patient.
Respirators are designed to protect the wearer from airborne particles. Studies have shown that they are at least 95% efficient against fine particles that are about 0.1 – 0.3 microns, assuming good fit on the wearer’s face.
Which Respirator will protect me from PM2.5?
We hear and read about ‘N95’ so much — are you sure you know what it means? Here’s a synopsis of what N95 certification means, from an independent testing centre in the USA:
“…If you are a manufacturer of respirators, one of the most important processes you must go through is to receive certification from the National Institute for Occupational Safety and Health (NIOSH). NIOSH respirator certification is necessary in order to label your respirator with one of the three ‘N’ certification categories: N95, N99 or N100. N95 respirators are used to filter contaminants such as dust, fumes, mists, as well as microbial agents including tuberculosis bacteria and flu virus. They are certified to filter greater than or equal to 95 percent of all challenged particles free of oil and greater than 0.3 microns in size. N99 respirators filter greater than or equal to 99 percent…”
In a nutshell, a respirator rated N95 filters out more than 95% of particles (PM) larger than 0.3 microns. This is a good thing, since most of air pollution effects are caused by particles with a size of 2.5 microns and smaller.
But here is an important point: almost every respirator you see on the market, except for some renowned companies like 3M, isn’t officially certified N95. Only the USA’s governmental agency NIOSH gives out the N95 certification, and if it’s not on their lists or database, then it’s not certified N95. Other countries have their own ratings which you may see on packages, such as the European EN149 FFP2 or BIS approved IS 9473:2002 FFP2 which are equivalent to N95.
-
